Renal Ultrasound
Introduction
Renal ultrasound is a fundamental imaging modality for evaluating kidney pathology due to:
- Excellent visualization of renal parenchyma and collecting system
- Real-time assessment of blood flow with Doppler
- No ionizing radiation or nephrotoxic contrast
- Bedside capability for critically ill patients
Limitations: Operator-dependent, limited evaluation of renal function, and restricted visualization in obese patients or those with abundant bowel gas.
Renal Anatomy
Normal Kidney Structure:
- Cortex: Hypoechoic to liver/spleen, contains glomeruli
- Medullary pyramids: More hypoechoic than cortex
- Sinus fat: Hyperechoic central area containing vessels and collecting system
- Pelvicalyceal system: Normally not distended
Normal Measurements:
- Length: 9-12 cm (adults)
- Cortical thickness: 7-10 mm
- Parenchymal thickness: 15-20 mm
- RI (resistive index): <0.7 (main renal artery)
Clinical Indications
1. Common Indications
- Flank/abdominal pain evaluation
- Hematuria assessment
- Renal function impairment
- Evaluation of hydronephrosis
- Suspected renal stones
2. Specific Clinical Scenarios
- Renal colic: Acute flank pain + hematuria
- Pyelonephritis: Fever + flank tenderness
- Renal failure: Elevated creatinine + oliguria
- Hypertension: Evaluation for renal artery stenosis
Scanning Technique
1. Patient Preparation
- Fasting: Not required but reduces bowel gas
- Bladder status: Full bladder helps evaluate distal ureters
- Positioning: Supine, decubitus, prone as needed
2. Equipment Settings
- Transducer: Curvilinear (2-5 MHz) for adults, higher frequency for children
- Depth: Adjust to include entire kidney and surrounding structures
- Harmonic imaging: Improves tissue contrast
- Doppler settings: Low PRF (800-1500 Hz) for renal vessels
3. Scanning Approach
- Systematic survey: Longitudinal and transverse views of both kidneys
- Coronal approach: Through liver/spleen as acoustic windows
- Posterior approach: Useful in obese patients
- Doppler assessment: Main renal artery, segmental arteries, and veins
Normal Sonographic Findings
1. Kidney Appearance
- Bean-shaped with smooth contours
- Cortex slightly hypoechoic to liver/spleen
- Medullary pyramids hypoechoic relative to cortex
- Central sinus hyperechoic due to fat
2. Vascular Anatomy
- Main renal artery visible at hilum
- Segmental arteries demonstrate low resistance flow
- Renal veins drain into IVC (right) or left renal vein crossing aorta
3. Variants
- Dromedary hump: Focal bulging of lateral border
- Column of Bertin: Cortical tissue extending into sinus
- Junctional parenchymal defect: Echogenic notch at fusion site

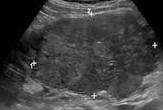
Normal Kidney
Demonstration of normal renal anatomy: cortex, medullary pyramids, and sinus fat. The cortex is slightly hypoechoic compared to adjacent spleen.

Renal Vasculature
Color Doppler showing normal renal artery and vein flow at the hilum with segmental branches.
Pathological Findings
1. Hydronephrosis
- Grade 1: Mild pelvic dilation only
- Grade 2: Pelvic and calyceal dilation
- Grade 3: Marked dilation with parenchymal thinning
- Causes: Stones, strictures, tumors, congenital
2. Renal Calculi
- Echogenic focus with posterior acoustic shadowing
- Twinkle artifact on color Doppler
- Secondary signs: Hydronephrosis, perinephric stranding
3. Pyelonephritis
- Focal or diffuse parenchymal hypo-/hyperechogenicity
- Loss of corticomedullary differentiation
- Possible complications: Abscess, emphysematous pyelonephritis
4. Renal Cysts
- Simple cysts: Anechoic, thin walls, posterior enhancement
- Complex cysts: Septations, calcifications, solid components
- Bosniak classification: Guides management
5. Renal Masses
- Angiomyolipoma: Hyperechoic fat-containing mass
- Renal cell carcinoma: Heterogeneous solid mass
- Transitional cell carcinoma: Filling defect in collecting system
6. Renal Failure
- Acute: Enlarged kidneys, echogenic cortex
- Chronic: Small kidneys, cortical thinning
- Doppler: Elevated resistive indices in parenchymal disease
7. Vascular Abnormalities
- Renal artery stenosis: Elevated velocities, tardus-parvus waveform
- Renal vein thrombosis: Absent venous flow, enlarged kidney
- AV fistula: High velocity turbulent flow

Hydronephrosis
- Grade 2 hydronephrosis
- Dilated pelvis and calyces
- Preserved parenchymal thickness

Renal Calculus
- Echogenic focus
- Posterior acoustic shadowing
- Mild hydronephrosis

Acute Pyelonephritis
- Focal hypoechoic area (arrows)
- Loss of corticomedullary differentiation
- Perinephric fat stranding
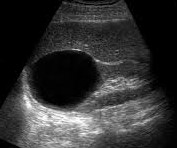
Simple Renal Cyst
- Anechoic lesion
- Thin imperceptible wall
- Posterior acoustic enhancement

Angiomyolipoma
- Well-circumscribed hyperechoic mass
- No acoustic shadowing
- Internal vascularity on Doppler
Renal Cell Carcinoma
- Heterogeneous solid mass (calipers)
- Distorting renal contour
- Internal vascularity
References
- American College of Radiology (ACR). (2023). ACR Appropriateness Criteria® Renal Failure. Journal of the American College of Radiology, 20(1S), S78-S92.
- Rumack, C. M., et al. (2023). Diagnostic Ultrasound (6th ed.). Elsevier.
- European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB). (2022). Guidelines on Renal Ultrasound. Ultraschall in der Medizin, 43(3), 261-279.
- O'Neill, W. C. (2023). Renal Ultrasound. In: Johnson, R. J., et al. (Eds.), Comprehensive Clinical Nephrology (7th ed., pp. 112-128). Elsevier.
- African Society of Uroradiology (ASUR). (2023). Consensus Guidelines on Renal Ultrasound in Tropical Settings. African Journal of Radiology, 28(1), 45-60.