Gastrointestinal Ultrasound
Introduction
Gastrointestinal ultrasound has become increasingly valuable for evaluating bowel pathology due to:
- Real-time assessment of bowel motility and peristalsis
- High-resolution evaluation of bowel wall layers
- Ability to assess vascular flow with Doppler
- No ionizing radiation, making it ideal for pediatric and pregnant patients
Limitations: Operator-dependent technique, limited by bowel gas, and restricted field of view compared to CT/MRI.
Gastrointestinal Anatomy
Bowel Wall Layers (from lumen outward):
- Mucosa: Hyperechoic inner layer
- Muscularis mucosae: Thin hypoechoic layer
- Submucosa: Thick hyperechoic layer
- Muscularis propria: Hypoechoic layer
- Serosa: Thin hyperechoic outer layer
Normal Measurements:
- Stomach wall: <5 mm (distended)
- Small bowel wall: <3 mm (distended)
- Colon wall: <4 mm (distended)
Clinical Indications
1. Common Indications
- Acute abdominal pain evaluation
- Suspected appendicitis
- Inflammatory bowel disease assessment
- Evaluation of bowel obstruction
- Suspected intussusception (especially in children)
2. Specific Clinical Scenarios
- Appendicitis: RLQ pain + rebound tenderness
- Crohn's disease: Chronic abdominal pain + diarrhea
- Bowel obstruction: Abdominal distension + vomiting
- Intussusception: Colicky pain + "red currant jelly" stools
Scanning Technique
1. Patient Preparation
- Fasting: 4-6 hours for upper GI evaluation
- Graded compression: Essential for appendiceal evaluation
- Positioning: Supine, then oblique/prone as needed
2. Equipment Settings
- Transducer: High-frequency linear (7-15 MHz) for superficial structures
- Depth: Adjust to include entire bowel wall and surrounding structures
- Harmonic imaging: Improves tissue contrast
- Doppler settings: Low PRF for slow flow detection
3. Scanning Approach
- Systematic survey: Begin in area of maximal tenderness
- Graded compression: Displace bowel gas for better visualization
- Dynamic assessment: Evaluate peristalsis and compressibility
- Water ingestion: Helpful for gastric evaluation
Normal Sonographic Findings
1. Bowel Wall Appearance
- Five distinct layers visible with high-frequency probes
- Peristalsis should be present in small bowel
- Haustra visible in colon
2. Appendix
- Blind-ending tubular structure arising from cecum
- Diameter <6 mm
- Compressible with no wall thickening
3. Specific Landmarks
- Pylorus: Thick muscular ring between stomach and duodenum
- Ileocecal valve: Prominent fold at terminal ileum-cecum junction
- Rectosigmoid: Evaluated with endocavitary probes
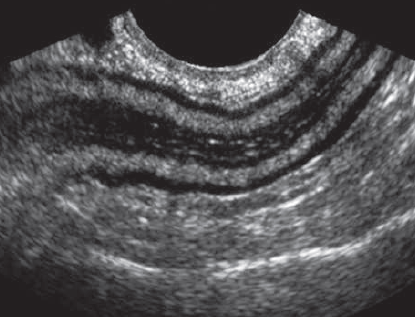
Normal Bowel Wall
Demonstration of the five sonographic layers of bowel wall (The muscle layers are hypoechoic. The submucosa and supericial mucosa layers are hyperechoic. There is a small amount of luid and air in the gut lumen).
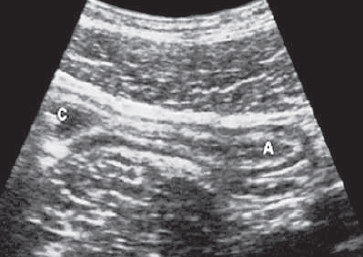
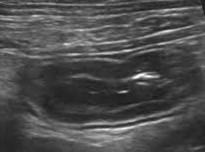
Normal Appendix
Compressible blind-ending tubular structure (A) measuring <6mm in diameter, araising from the caecum (C).
Pathological Findings
1. Appendicitis
- Direct signs: Non-compressible, blind-ending tube >6mm diameter
- Wall changes: Thickened (>3mm), hyperemic on Doppler
- Secondary signs: Periappendiceal fat inflammation, free fluid
2. Inflammatory Bowel Disease
- Crohn's disease: Segmental wall thickening (>4mm), loss of stratification
- Ulcerative colitis: Diffuse wall thickening with preserved layers
- Complications: Fistulas, abscesses, strictures
3. Bowel Obstruction
- Mechanical obstruction: Dilated proximal loops (>3cm), collapsed distal loops
- Paralytic ileus: Diffuse bowel dilation with absent peristalsis
- Closed-loop obstruction: U-shaped dilated loop with mesenteric congestion
4. Intussusception
- Target sign: Concentric rings on transverse view
- Pseudokidney sign: Longitudinal appearance
- Lead point: May be visible in pathological cases
5. Diverticulitis
- Focal bowel wall thickening at site of diverticulum
- Inflamed diverticulum appears as hyperechoic focus
- Pericolic fat inflammation and possible abscess
6. Neoplasms
- GIST: Hypoechoic mass arising from muscularis propria
- Adenocarcinoma: Irregular hypoechoic wall thickening
- Lymphoma: Marked hypoechoic wall thickening with preserved layers

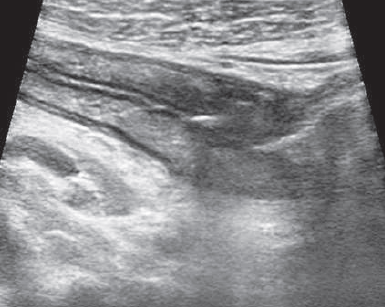
Acute Appendicitis
- Non-compressible appendix (calipers)
- Wall thickening (>3mm)
- Surrounding hyperechoic fat
Crohn's Disease
- Segmental wall thickening
- Loss of normal stratification
- Mesenteric fat hypertrophy

Intussusception
- Target sign (transverse view)
- Multiple concentric rings
- Mesenteric fat dragged in (arrow)
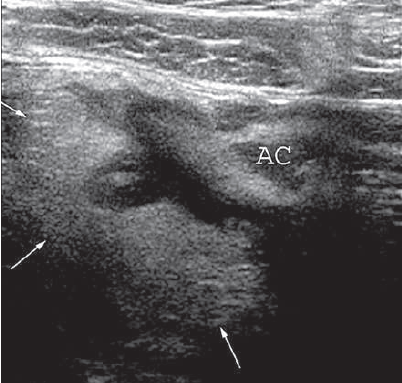
Diverticulitis
- Focal wall thickening
- Inflamed diverticulum, arises from the lateral wall of the ascending colon (AC)
- Pericolic fat inflammation (arrows)

Gastrointestinal Stromal Tumor
- Hypoechoic mass (yellow arriow) arising from bowel wall
- Internal vascularity on Doppler
Bowel Lymphoma
- Marked hypoechoic wall thickening (arrows)
- Preserved wall layers
- Associated lymphadenopathy (Not shown)
References
- American College of Radiology (ACR). (2023). ACR Appropriateness Criteria® Right Lower Quadrant Pain. Journal of the American College of Radiology, 20(1S), S78-S92.
- Kratzer, W., et al. (2022). Atlas of Gastrointestinal Ultrasound (2nd ed.). Thieme.
- Nylund, K., et al. (2021). EFSUMB Recommendations for Gastrointestinal Ultrasound. Ultraschall in der Medizin, 42(3), 261-279.
- Wilson, S. R. (2022). The Gastrointestinal Tract. In: Rumack, C. M., & Levine, D. (Eds.), Diagnostic Ultrasound (6th ed., pp. 345-412). Elsevier.
- European Society of Gastrointestinal and Abdominal Radiology (ESGAR). (2023). Consensus Guidelines on Bowel Ultrasound in Inflammatory Bowel Disease. European Radiology, 33(1), 255-270.