Ultrasound of Inflammatory Bowel Disease
Introduction
Ultrasound has emerged as a valuable tool for evaluating inflammatory bowel disease (IBD), offering a non-invasive, radiation-free method for assessing disease activity, complications, and treatment response. This article focuses on the sonographic features of Crohn's disease and ulcerative colitis, the two main forms of IBD.
Key Advantages of Ultrasound in IBD:
- No ionizing radiation (important for young patients requiring repeated imaging)
- Real-time assessment of peristalsis and compressibility
- Evaluation of extramural complications (abscesses, fistulas)
- Bedside availability and low cost
- Ability to guide interventions (drainage, biopsies)
1. Crohn's Disease
A chronic transmural inflammatory condition that can affect any part of the gastrointestinal tract, most commonly the terminal ileum and colon.
Pathological Features
- Skip lesions with normal intervening bowel
- Transmural inflammation leading to strictures and fistulas
- Mesenteric fat hypertrophy ("creeping fat")
- Lymphoid hyperplasia and granuloma formation
Ultrasound Findings
- Bowel wall thickening (>3mm in small bowel, >4mm in colon)
- Stratification loss (disruption of normal wall layers)
- Mesenteric fat hypertrophy (hyperechoic fat surrounding bowel)
- Increased vascularity on color Doppler (active inflammation)
- Strictures (prestenotic dilation, reduced peristalsis)
- Fistulas and abscesses (hypoechoic tracts/collections)
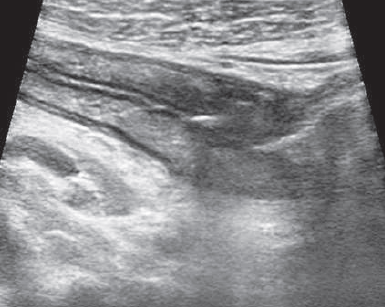
Terminal Ileum in Crohn's
- Marked wall thickening (7.2mm)
- Loss of normal stratification
- Surrounding hyperechoic fat

Crohn's Stricture
- Narrowed lumen with wall thickening
- Pre-stenotic dilation
2. Ulcerative Colitis
A chronic mucosal inflammatory condition limited to the colon, always starting in the rectum and extending proximally in a continuous fashion.
Pathological Features
- Continuous mucosal inflammation (no skip lesions)
- Superficial ulcers and pseudopolyps
- Mucosal atrophy in chronic disease
- No transmural inflammation or fistulas
Ultrasound Findings
- Colonic wall thickening (typically 5-10mm in active disease)
- Preserved stratification (unlike Crohn's)
- Mucosal irregularity (pseudopolyps, ulcers)
- Pericolic fat inflammation (mild compared to Crohn's)
- Haustra loss in chronic cases
- Backwash ileitis (terminal ileum involvement in pancolitis)
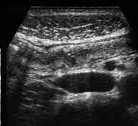
Ulcerative Colitis
- Diffuse colonic wall thickening
- Preserved wall layers
- Mucosal irregularity
Chronic UC
- Featureless colon
- Loss of haustration
- Narrow lumen
3. Disease Activity Assessment
Ultrasound can help differentiate active inflammation from chronic fibrotic changes, guiding treatment decisions.
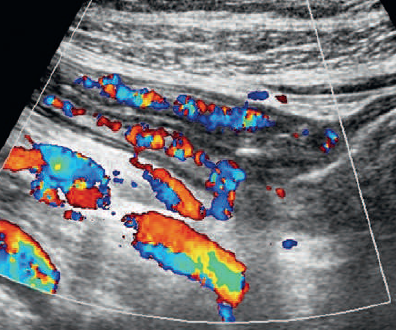
Features Suggesting Active Inflammation
- Increased vascularity on color Doppler
- Hypoechoic wall thickening (edema)
- Perienteric fat inflammation (hyperechoic fat)
- Lymph nodes enlargement (short axis >5mm)
- Free fluid adjacent to affected bowel
Features Suggesting Chronic/Fibrotic Disease
- Hyperechoic wall thickening (fibrosis)
- Strictures without hyperemia
- Reduced peristalsis
- Prestenotic dilation
- Absence of vascularity in thickened segments
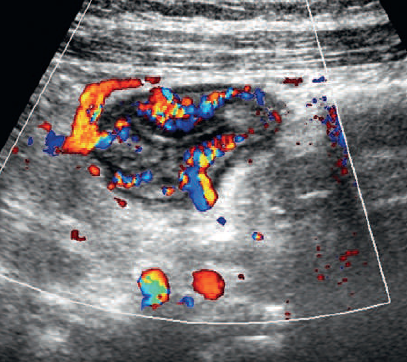
Active Crohn's
- Hypoechoic wall thickening
- Marked hyperemia on Doppler
- Surrounding fat inflammation
Fibrotic Stricture
- Hyperechoic wall thickening
- No vascularity on Doppler
- Prestenotic dilation
4. IBD Complications
Ultrasound is particularly valuable for detecting extramural complications of IBD.
Common Complications
- Abscesses:
- Hypo/anechoic collections with thick walls
- May contain debris or gas (hyperechoic foci with shadowing)
- Fistulas:
- Hypoechoic tracts connecting bowel to other structures
- May show gas bubbles (hyperechoic foci with reverberation)
- Strictures:
- Fixed luminal narrowing with prestenotic dilation
- Reduced/absent peristalsis at stricture site
- Toxic megacolon (in UC):
- Colonic dilation >6cm
- Thin, featureless walls
- Absent haustration

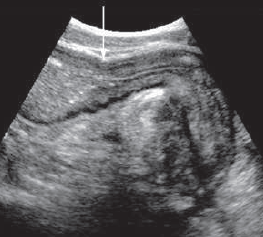
Abscess
- Hypoechoic collection with debris
- Thick irregular walls
- Adjacent to inflamed bowel
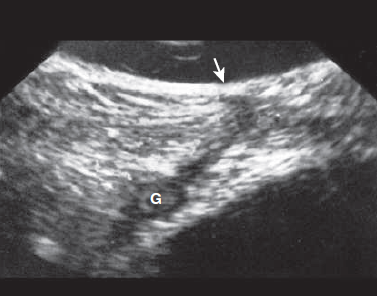
Enterocutaneous Fistula
- Hypoechoic tract
- Connecting bowel (G) to skin surface (arrow)
- Gas bubbles within tract
5. Differential Diagnosis
Several conditions can mimic IBD on ultrasound:
| Condition | Key Differentiating Features |
|---|---|
| Infectious colitis | Often more diffuse, no fat wrapping, clinical history |
| Diverticulitis | Focal pericolonic inflammation, diverticula present |
| Ischemic colitis | Segmental, reduced vascularity, clinical context |
| Lymphoma | Marked hypoechoic thickening, no hyperemia |
| Tuberculosis | Ileocecal involvement, necrotic lymph nodes |
| NSAID enteropathy | Diaphragm-like strictures, no fat wrapping |
References
- Maconi G, et al. EFSUMB Recommendations and Clinical Guidelines for Intestinal Ultrasound (GIUS) in Inflammatory Bowel Diseases. Ultraschall Med. 2018;39(3):304-317.
- Nylund K, et al. EFSUMB Recommendations and Guidelines for Gastrointestinal Ultrasound. Ultraschall Med. 2017;38(3):e1-e15.
- Panes J, et al. Imaging techniques for assessment of inflammatory bowel disease: joint ECCO and ESGAR evidence-based consensus guidelines. J Crohns Colitis. 2013;7(7):556-585.
- Kucharzik T, et al. Ultrasound in Inflammatory Bowel Disease - So Far We Are? Clin Gastroenterol Hepatol. 2022;20(1):1-12.
- Allocca M, et al. Use of Intestinal Ultrasound to Monitor Crohn's Disease Activity. Clin Gastroenterol Hepatol. 2017;15(4):535-542.
- Maaser C, et al. Intestinal ultrasound for monitoring therapeutic response in patients with ulcerative colitis: results from the TRUST&UC study. Gut. 2020;69(9):1629-1636.
- Ripollés T, et al. Contrast-enhanced ultrasound in the differentiation between phlegmon and abscess in Crohn's disease and other abdominal conditions. Eur J Radiol. 2013;82(10):e525-e531.
- Dietrich CF, et al. Ultrasound of the colon in inflammatory bowel disease. World J Gastroenterol. 2021;27(20):2473-2495.
- Rumack CM, Levine D. Diagnostic Ultrasound. 5th ed. Elsevier; 2018.
- American Institute of Ultrasound in Medicine (AIUM). AIUM practice guideline for the performance of gastrointestinal ultrasound examination. J Ultrasound Med. 2021;40(5):895-903.