Pelvic Inflammatory Disease (PID)
Introduction
Pelvic Inflammatory Disease (PID) is an infection of the female upper genital tract including the endometrium, fallopian tubes, ovaries, and adjacent pelvic structures. Ultrasound plays a crucial role in diagnosis and assessment of complications. This article details the sonographic appearance of PID with emphasis on:
- Acute salpingitis - Inflammation of fallopian tubes
- Pyosalpinx - Pus-filled dilated tube
- Tubo-ovarian abscess (TOA) - Advanced infection with complex adnexal mass
- Oophoritis - Ovarian inflammation
- Endometritis - Uterine lining inflammation
- Pelvic peritonitis - Inflammation extending beyond reproductive organs
1. Acute Salpingitis
Early stage PID characterized by fallopian tube inflammation without significant fluid accumulation.
Pathophysiology
Ascending infection (typically N. gonorrhoeae or C. trachomatis) → endosalpingeal edema → ciliary dysfunction → inflammatory exudate.
Ultrasound Findings
- Tubal wall thickening (>5mm)
- Incomplete septae within dilated tube ("cogwheel sign")
- Hypervascularity on Doppler imaging
- Pelvic free fluid (often complex)
- Ovarian stromal edema (enlarged, hypoechoic ovaries)

Acute Salpingitis
- Thickened tubal walls (>5mm)
- Incomplete septations
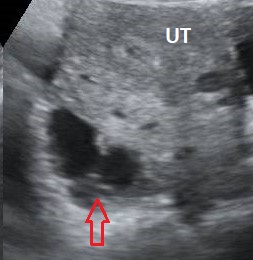
Cogwheel Sign
- Transverse view of inflamed tube (red arrow)
- Characteristic "cogwheel" appearance
- UT is the uterus
2. Pyosalpinx
Advanced salpingitis with pus accumulation in the fallopian tube lumen.
Clinical Features
Severe pelvic pain, fever, cervical motion tenderness. Risk factors include multiple sexual partners, IUD use, and prior PID.
Ultrasound Findings
- Dilated tube (>10mm diameter) with thick walls
- Low-level internal echoes (pus content)
- "Beads-on-a-string" sign - hyperechoic mucosal folds in distended tube
- Fluid-debris level (pathognomonic)
- Increased vascularity in tubal walls

Pyosalpinx
- Dilated tube with thick walls
- Low-level internal echoes
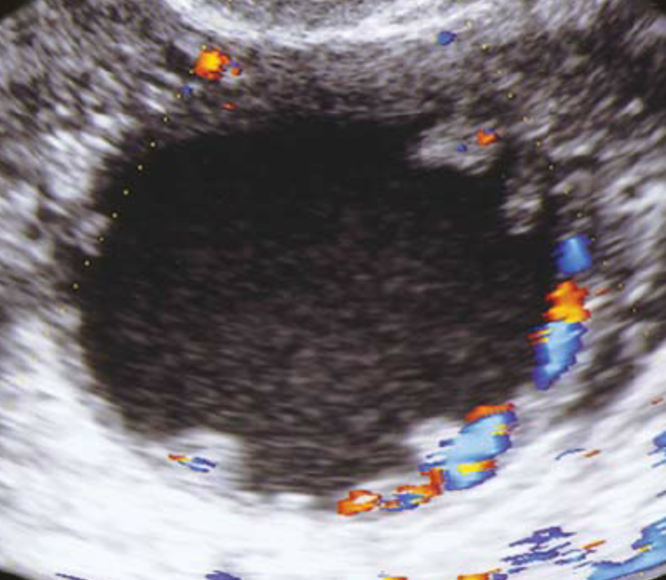
Beads-on-a-string Sign
- Hyperechoic mucosal folds
- Distended fallopian tube
- Hypervascularity on color Doppler
3. Tubo-Ovararian Abscess (TOA)
Most severe form of PID where infection spreads beyond tubes to involve ovaries and adjacent structures.
Ultrasound Findings
- Complex adnexal mass with thick irregular walls
- Septations and internal debris
- Indistinct ovarian borders (ovary incorporated into mass)
- Gas bubbles (hyperechoic foci with dirty shadowing)
- Pelvic fat stranding (hyperechoic peritoneum)
Clinical Significance
Requires IV antibiotics ± drainage. Rupture can lead to life-threatening sepsis.

Tubo-Ovarian Abscess
- Complex adnexal mass
- Thick irregular walls

TOA with Gas
- Hyperechoic gas foci
- "Dirty" posterior shadowing
4. Oophoritis
Isolated ovarian inflammation, often coexisting with salpingitis in PID.
Ultrasound Findings
- Ovarian enlargement (volume >10cm³)
- Stromal edema (diffuse hypoechogenicity)
- Hypervascularity on Doppler ("fire ring" pattern)
- Follicular wall thickening (>3mm)
- Periovarian fat stranding (hyperechoic surrounding tissue)
Clinical Pearls
- Often bilateral but may be asymmetric
- Differentiate from ovarian torsion (preserved venous flow in oophoritis)
- May progress to TOA if untreated
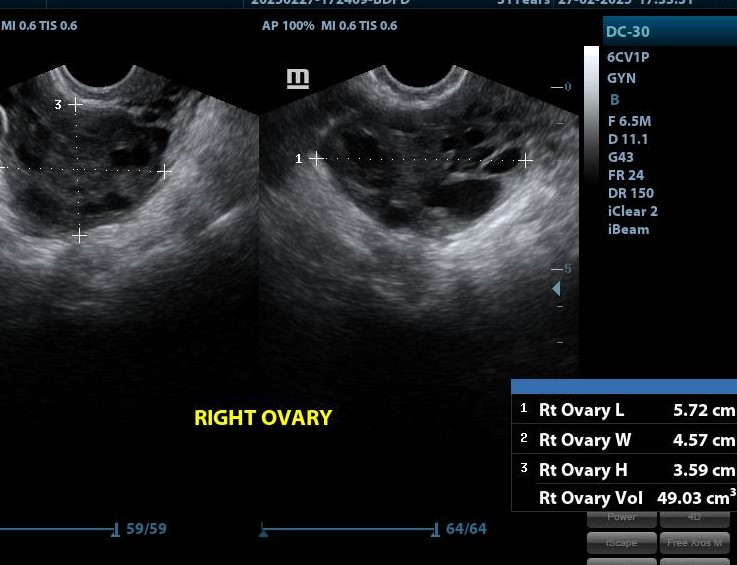
Oophoritis with Stromal Edema
- Enlarged ovary (49.03cm³)
- Diffuse hypoechoic stroma
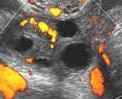
Oophoritis Hypervascularity
- "Fire ring" pattern on Doppler
- Resistive Index <0.5
5. Endometritis
Inflammation of the endometrial lining, often coexisting with salpingitis.
Ultrasound Findings
- Endometrial thickening (>8mm in proliferative phase)
- Intrauterine fluid (complex echogenicity)
- Air in endometrial cavity (postpartum cases)
- Hypervascular endometrium on Doppler
- Irregular endometrial-myometrial interface
Risk Factors
Recent childbirth, miscarriage, IUD insertion, or instrumentation of uterus.

Endometritis
- Thickened endometrium
- Intrauterine fluid (asterisk)

Endometritis with Air
- Hyperechoic air foci
- Postpartum patient
6. Fitz-Hugh-Curtis Syndrome
Perihepatitis complication of PID causing right upper quadrant pain ("violin string" adhesions).
Ultrasound Findings
- Perihepatic fluid (often complex)
- Thickened gallbladder wall (reactive change)
- Hepatic capsular enhancement on Doppler
- Adhesions between liver and diaphragm
Clinical Pearls
Consider in young women with RUQ pain + cervical motion tenderness. Differentiate from cholecystitis.

Fitz-Hugh-Curtis
- Perihepatic fluid (red arrow)
- Thickened hepatic capsule

Violin String Adhesions
- Laparoscopic view
- Thin fibrous bands
Differential Diagnosis
| Condition | Key Differentiating Features |
|---|---|
| Ectopic pregnancy | Positive β-hCG, decidual reaction, no fever |
| Endometriosis | Cyclic pain, "kissing ovaries," no infection signs |
| Ovarian torsion | Absent venous flow, twisted vascular pedicle |
| Appendicitis | Non-gynecologic pain, dilated appendix |
| Diverticulitis | Colonic wall thickening, pericolic fat stranding |
Management Guidelines
Mild PID
- Outpatient treatment
- Ceftriaxone 250mg IM + Doxycycline 100mg BID x14d
- Metronidazole 500mg BID x14d (if anaerobes suspected)
Severe PID/TOA
- Hospital admission
- IV Cefoxitin/Ertapenem + Doxycycline
- Ultrasound-guided drainage if >5cm
- Surgical intervention if rupture suspected
References
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021;70(4):1-187. doi:10.15585/mmwr.rr7004a1
- Romero R, Espinoza J, Mazor M. Can endometrial infection/inflammation explain implantation failure, spontaneous abortion, and preterm birth after in vitro fertilization? Fertil Steril. 2004;82(4):799-804. doi:10.1016/j.fertnstert.2004.05.076
- Rezvani M, Shaaban AM. Fallopian tube disease in the nonpregnant patient. Radiographics. 2011;31(2):527-548. doi:10.1148/rg.312105090
- Sam JW, Jacobs JE, Birnbaum BA. Spectrum of CT findings in acute pyogenic pelvic inflammatory disease. Radiographics. 2002;22(6):1327-1334. doi:10.1148/rg.226025040
- Kurman RJ, Ellenson LH, Ronnett BM. Blaustein's Pathology of the Female Genital Tract. 7th ed. Springer; 2019.
- Kaakaji Y, Nghiem HV, Nodell C, Winter TC. Sonography of obstetric and gynecologic emergencies: Part I, Obstetric emergencies. AJR Am J Roentgenol. 2000;174(3):641-649. doi:10.2214/ajr.174.3.1740641
- Timor-Tritsch IE, Lerner JP, Monteagudo A, Murphy KE, Heller DS. Transvaginal sonographic markers of tubal inflammatory disease. Ultrasound Obstet Gynecol. 1998;12(1):56-66. doi:10.1046/j.1469-0705.1998.12010056.x
- American Institute of Ultrasound in Medicine (AIUM). AIUM practice guideline for the performance of pelvic ultrasound examinations. J Ultrasound Med. 2020;39(6):E41-E46. doi:10.1002/jum.15235
- Centers for Disease Control and Prevention. Pelvic Inflammatory Disease (PID) - CDC Fact Sheet. Accessed May 19, 2025. https://www.cdc.gov/std/pid/stdfact-pid.htm
- Mitchell C, Prabhu M. Pelvic inflammatory disease: current concepts in pathogenesis, diagnosis and treatment. Infect Dis Clin North Am. 2013;27(4):793-809. doi:10.1016/j.idc.2013.08.004