Uterus Ultrasound
Introduction
Uterine ultrasound is the primary imaging modality for evaluating gynecological pathology due to:
- Excellent visualization of uterine anatomy and layers
- Real-time assessment of endometrial changes
- No ionizing radiation
- Ability to assess vascularity with Doppler
- Cost-effectiveness in resource-limited settings
Limitations: Operator-dependent, limited evaluation of deep myometrial invasion compared to MRI, and restricted visualization in patients with large body habitus.
Uterine Anatomy
Layers of the Uterus:
- Endometrium: Inner mucosal layer, echogenicity varies with menstrual cycle
- Myometrium: Middle muscular layer, homogeneous mid-level echogenicity
- Serosa: Outer layer, thin hyperechoic line
Normal Measurements:
- Nulliparous: 6-8 cm length, 3-5 cm width, 2-3 cm AP
- Multiparous: 8-10 cm length, 4-6 cm width, 3-5 cm AP
- Postmenopausal: ≤6 cm length, ≤2 cm AP (without HRT)
- Endometrial thickness: Varies with cycle (4-16 mm proliferative/secretory, ≤4 mm postmenopausal)
Clinical Indications
1. Common Indications
- Abnormal uterine bleeding
- Pelvic pain evaluation
- Suspected fibroids or adenomyosis
- Infertility workup
- Postmenopausal bleeding
- Congenital uterine anomalies
2. Specific Clinical Scenarios
- Fibroids: Menorrhagia, bulk symptoms, infertility
- Adenomyosis: Dysmenorrhea, menorrhagia, enlarged uterus
- Endometrial cancer: Postmenopausal bleeding, thickened endometrium
- Congenital anomalies: Recurrent pregnancy loss, infertility
Scanning Technique
1. Patient Preparation
- Transabdominal: Full bladder required (pushes bowel away)
- Transvaginal: Empty bladder, appropriate consent
- Positioning: Supine for transabdominal, lithotomy for transvaginal
- Timing: Days 5-10 of cycle for optimal endometrial assessment
2. Equipment Settings
- Transducer: Curvilinear (3-5 MHz) for transabdominal, endovaginal (5-9 MHz) for TVS
- Depth: Adjust to include entire uterus and adnexa
- Harmonic imaging: Improves tissue contrast
- Doppler settings: Low PRF (800-1500 Hz) for uterine vessels
3. Scanning Approach
- Systematic survey: Sagittal and transverse sweeps
- Endometrial assessment: Measure maximal thickness in sagittal plane
- Myometrial evaluation: Assess for focal lesions and vascularity
- 3D ultrasound: For congenital anomalies (when available)
Normal Sonographic Findings
1. Uterine Appearance
- Pear-shaped organ with smooth contours
- Homogeneous myometrial echotexture
- Endometrial changes with menstrual cycle:
- Menstrual: Thin, irregular hyperechoic line
- Proliferative: Triple-layer appearance
- Secretory: Thick, hyperechoic uniform
2. Vascular Anatomy
- Minimal flow in myometrium on color Doppler
- Arcuate vessels at outer myometrium
- Subendometrial vascular ring in secretory phase
3. Variants
- Retroverted uterus: Fundus points posteriorly
- Myometrial cysts: Small anechoic areas in myometrium
- Endometrial fluid: Small amount in postmenopausal women
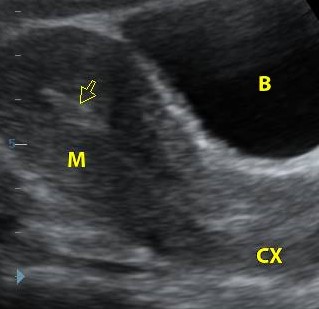
Normal Uterus (Sagittal)
Midline sagittal view showing normal endometrial stripe (arrow), myometrium (M), and cervix (CX). Bladder (B) is anterior.
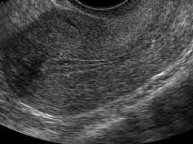
Endometrial Phases
1. Proliferative phase with triple-layer appearance.
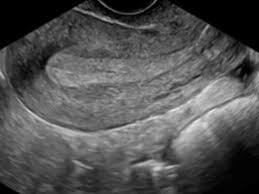
Endometrial Phases
2. Secretory phase with thick hyperechoic endometrium.
Pathological Findings
1. Leiomyomas (Fibroids)
- Well-circumscribed, round masses
- Variable echogenicity: hypoechoic (most common), hyperechoic, or mixed
- Shadowing with calcification
- Peripheral vascularity on Doppler
- Subtypes: submucosal, intramural, subserosal, pedunculated
2. Adenomyosis
- Diffuse uterine enlargement
- Heterogeneous myometrium with striations
- Myometrial cysts (1-5 mm)
- Poorly defined lesion borders
- Increased vascularity throughout myometrium
3. Endometrial Polyps
- Hyperechoic focal endometrial thickening
- Feeding vessel on Doppler ("pedicle artery" sign)
- May have cystic spaces
- Persistent despite menstrual shedding
4. Endometrial Carcinoma
- Thickened, irregular endometrium (>4mm postmenopausal)
- Heterogeneous echotexture
- Myometrial invasion: irregular endometrium-myometrium interface
- Increased vascularity with chaotic flow
5. Congenital Uterine Anomalies
- Septate uterus: Fundal indentation <1cm, single endometrial cavity
- Bicornuate uterus: Fundal indentation >1cm, two endometrial cavities
- Didelphys uterus: Complete duplication with two cervices
- Unicornuate uterus: Banana-shaped single horn
6. Postpartum Complications
- Retained products: Heterogeneous endometrial mass with vascularity
- Placenta accreta: Loss of retroplacental clear space, lacunae
- Endometritis: Endometrial fluid with gas shadows

Uterine Fibroid
- Well-defined hypoechoic mass (arrow)
- Posterior acoustic shadowing
- Peripheral vascularity on Doppler

Adenomyosis
- Diffuse uterine enlargement
- Heterogeneous myometrium
- Myometrial cysts

Endometrial Polyp
- Focal endometrial thickening (P)
- Single feeding vessel ("pedicle sign")
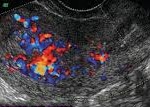
Endometrial Carcinoma
- Thickened heterogeneous endometrium (E)
- Irregular endometrium-myometrium interface
- Increased chaotic vascularity
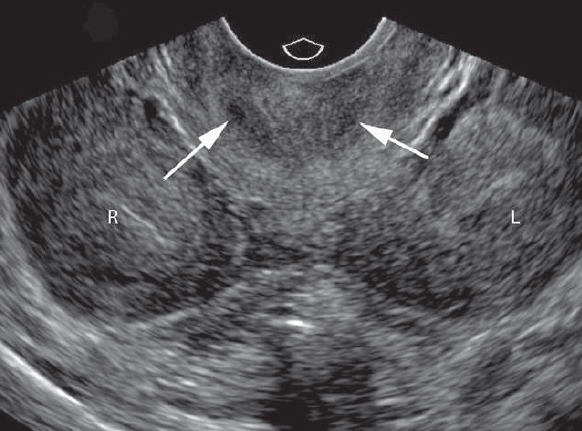
Uterus didelphys
- Two separate uterine cavities (R & L)
- Two cervices (arrows).
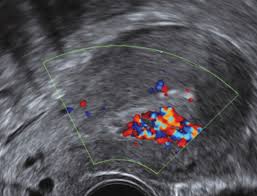
Retained Products
- Heterogeneous endometrial mass (R)
- Increased vascularity on Doppler
- Clinical history of recent delivery
References
- American College of Radiology (ACR). (2023). ACR Appropriateness Criteria® Abnormal Uterine Bleeding. Journal of the American College of Radiology, 20(1S), S78-S92.
- Salen, P., et al. (2023). Gynecologic Ultrasound (4th ed.). Elsevier.
- European Society of Urogenital Radiology (ESUR). (2022). Guidelines on Gynecological Ultrasound. European Radiology, 33(3), 261-279.
- Timor-Tritsch, I. E. (2023). Uterine Ultrasound. In: Rumack, C. M., & Levine, D. (Eds.), Diagnostic Ultrasound (6th ed., pp. 112-128). Elsevier.
- African Society of Uroradiology (ASUR). (2023). Consensus Guidelines on Gynecological Ultrasound in African Populations. African Journal of Radiology, 28(1), 45-60.