Prostate Ultrasound
Introduction
Prostate ultrasound is an essential imaging modality for evaluating prostate pathology due to:
- Detailed visualization of prostate anatomy and zonal architecture
- Real-time guidance for biopsies and interventions
- No ionizing radiation
- Ability to assess vascularity with Doppler
Limitations: Operator-dependent, limited evaluation of extracapsular extension compared to MRI, and restricted visualization in patients with dense calcifications.
Prostate Anatomy
Zonal Anatomy:
- Peripheral zone: 70% of glandular tissue, hypoechoic, site of most cancers
- Central zone: 25% of gland, hyperechoic, rarely involved by cancer
- Transition zone: 5% (young men), site of BPH, mixed echogenicity
- Anterior fibromuscular stroma: Hypoechoic, non-glandular
Normal Measurements:
- Width: 4-5 cm (transverse)
- Height: 2.5-3 cm (sagittal)
- Length: 3-4 cm (AP)
- Volume: 20-30 mL (calculated as L×W×H×0.52)
Clinical Indications
1. Common Indications
- Evaluation of prostate size in BPH
- Suspected prostate cancer
- Elevated PSA levels
- Prostatitis assessment
- Guidance for biopsy and interventions
2. Specific Clinical Scenarios
- BPH: LUTS, urinary retention
- Prostate cancer: Elevated PSA, abnormal DRE
- Prostatitis: Pelvic pain, fever, dysuria
- Infertility: Evaluation of seminal vesicles
Scanning Technique
1. Patient Preparation
- Transrectal (TRUS): Bowel prep (enema), antibiotic prophylaxis
- Transabdominal: Full bladder required
- Positioning: Left lateral decubitus for TRUS, supine for transabdominal
2. Equipment Settings
- Transducer: Endocavitary (5-10 MHz) for TRUS, curvilinear (3-5 MHz) for transabdominal
- Depth: Adjust to include entire prostate and seminal vesicles
- Harmonic imaging: Improves tissue contrast
- Doppler settings: Low PRF (800-1500 Hz) for prostatic vessels
3. Scanning Approach
- Systematic survey: Sagittal and transverse sweeps
- Zonal evaluation: Assess peripheral, central and transition zones
- Volume measurement: Ellipsoid formula (L×W×H×0.52)
- Biopsy guidance: 12-core systematic sampling
Normal Sonographic Findings
1. Prostate Appearance
- Symmetrical, triangular/oval shape
- Homogeneous echotexture with smooth capsule
- Peripheral zone slightly hypoechoic compared to central zone
- Seminal vesicles: Paired, hypoechoic structures above prostate
2. Vascular Anatomy
- Minimal flow on color Doppler
- Symmetrical capsular and urethral arteries
- No hypervascular foci in normal prostate
3. Variants
- Corpora amylacea: Small echogenic foci, no shadowing
- Ejaculatory duct cysts: Small midline cystic structures
- BPH nodules: Early transition zone nodules
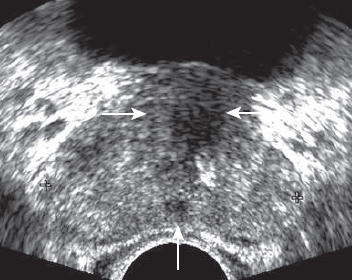
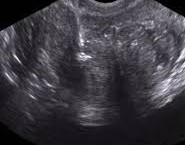
Normal Prostate (TRUS)
Transverse view at midgland level. Note the normal hypoechoic muscular internal urethral sphincter (horizontal arrows) and the ejaculatory ducts (vertical arrow).
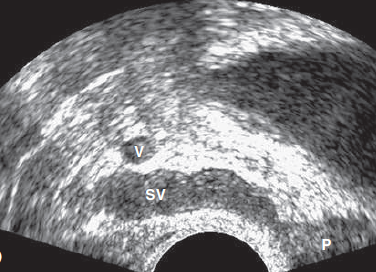
Normal Seminal Vesicles
Sagittal view showing hypoechoic seminal vesicles (SV) superior to the prostate (P) with normal vascularity on Doppler.
Pathological Findings
1. Benign Prostatic Hyperplasia (BPH)
- Enlarged transition zone (>30 mL volume)
- Heterogeneous nodules with cystic changes
- Compressed peripheral zone ("surgical capsule")
- Possible post-void residual urine
2. Prostate Cancer
- Hypoechoic nodule in peripheral zone (70% of cases)
- Asymmetrical capsular bulging
- Increased vascularity on Doppler
- Possible seminal vesicle invasion
3. Prostatitis
- Diffuse or focal hypoechogenicity
- Increased vascularity on Doppler
- Possible abscess formation (hypoechoic area with debris)
- Periprostatic fat inflammation
4. Prostate Cysts
- Utricular cysts: Midline, may communicate with urethra
- Müllerian duct cysts: Extend above prostate
- Retention cysts: Small, multiple in BPH
5. Calcifications
- Common in BPH and chronic prostatitis
- Echogenic foci with posterior shadowing
- Corpora amylacea: Small, non-shadowing
6. Post-Biopsy Changes
- Focal hematomas (hypoechoic areas)
- Increased vascularity at biopsy sites
- Possible abscess formation (rare)

Benign Prostatic Hyperplasia
- Enlarged transition zone (TZ)
- Heterogeneous nodular appearance
- Compressed peripheral zone (PZ)
Prostate Cancer
- Hypoechoic nodule (arrows) in peripheral zone
- Irregular capsular contour
- Increased vascularity on Doppler
Acute Prostatitis
- Diffuse hypoechogenicity
- Increased vascularity
- Swollen seminal vesicles

Prostate Cyst
- Well-defined anechoic lesion
- No internal vascularity
- Posterior acoustic enhancement
Prostate Calcifications
- Multiple echogenic foci
- Posterior acoustic shadowing
- Typical in chronic prostatitis

Post-Biopsy Changes
- Hypoechoic hematoma
- Mild increased vascularity
- Intact prostatic capsule
References
- American College of Radiology (ACR). (2023). ACR Appropriateness Criteria® Prostate Cancer Detection. Journal of the American College of Radiology, 20(1S), S78-S92.
- Sidhu, P. S., et al. (2023). Clinical Ultrasound (4th ed.). Elsevier.
- European Society of Urogenital Radiology (ESUR). (2022). Guidelines on Prostate Ultrasound. European Radiology, 33(3), 261-279.
- Rifkin, M. D. (2023). Prostate Ultrasound. In: Rumack, C. M., & Levine, D. (Eds.), Diagnostic Ultrasound (6th ed., pp. 112-128). Elsevier.
- African Society of Uroradiology (ASUR). (2023). Consensus Guidelines on Prostate Ultrasound in African Populations. African Journal of Radiology, 28(1), 45-60.