Appendicitis: Imaging Diagnosis
Introduction
Appendicitis is the most common abdominal surgical emergency worldwide, with a lifetime risk of approximately 7%. Imaging plays a crucial role in diagnosis, particularly in atypical presentations. This article details the imaging features of appendicitis across modalities, with emphasis on ultrasound (first-line in children and pregnant women) and CT (gold standard in adults).
- Ultrasound features - Graded compression technique findings
- CT features - Multi-detector CT diagnostic criteria
- Complicated appendicitis - Findings of perforation/abscess
- Differential diagnosis - Mimickers of appendicitis
- Special populations - Pediatric, pregnant, and elderly patients
1. Ultrasound Features
Graded compression ultrasound is the initial imaging modality of choice for children and pregnant patients with suspected appendicitis.
Technique
High-frequency linear transducer (5-12MHz) with gradual compression in RLQ to displace bowel gas and identify the appendix.
Diagnostic Criteria
- Non-compressible tubular structure >6mm diameter
- Target sign - concentric wall layers
- Wall thickening (>3mm) with hyperemia on Doppler
- Periappendiceal fat hyperechogenicity (inflammation)
- Appendicolith - echogenic focus with posterior shadowing

Acute Appendicitis
- Non-compressible dilated appendix (7.3mm)
- Wall thickening and hyperemia
Appendicolith
- Echogenic focus with clean shadowing
- Surrounding hypoechoic fluid
2. CT Features
Contrast-enhanced CT is the gold standard for diagnosing appendicitis in adults, with sensitivity of 94-98% and specificity of 95%.
Protocol
Multi-detector CT with IV contrast (oral/rectal contrast optional). 2-3mm reconstructions.
Diagnostic Criteria
- Appendix diameter >6mm with wall thickening
- Periappendiceal fat stranding (most sensitive sign)
- Appendiceal wall enhancement with IV contrast
- Appendicolith - calcified focus in lumen
- Adjacent fascial thickening
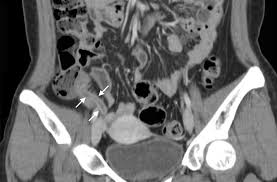
Acute Appendicitis
- Dilated fluid-filled appendix (arrows)
- Surrounding fat stranding

Appendicolith
- Calcified focus (arrow) within dilated appendix
- Adjacent inflammatory changes
3. Complicated Appendicitis
Findings suggesting perforation, abscess formation, or peritonitis that may alter surgical approach.
Imaging Findings
- Focal defect in appendiceal wall (direct sign of perforation)
- Extraluminal air (pneumoperitoneum rare)
- Phlegmon - ill-defined soft tissue mass
- Abscess - fluid collection with enhancing rim
- Extensive free fluid with debris
Management Implications
Perforation may require percutaneous drainage prior to interval appendectomy. Free perforation with peritonitis needs emergent surgery.

Perforated Appendicitis
- Focal wall defect
- Surrounding abscess formation

Appendiceal Abscess
- Fluid collection with enhancing rim
- Adjacent inflammatory changes
4. Differential Diagnosis
Several conditions can mimic appendicitis clinically and radiologically.
Common Mimickers
- Mesenteric adenitis - enlarged lymph nodes, normal appendix
- Omental infarction - fatty mass with inflammatory changes
- Diverticulitis - left-sided in adults, right-sided cecal in elderly
- Gynecological pathology - ovarian torsion, PID, ectopic pregnancy
- Crohn's disease - terminal ileum involvement
Mesenteric Adenitis
- Cluster of enlarged mesenteric nodes
- Normal appendix

Omental Infarction
- Fat density mass with inflammatory stranding
- No identifiable appendix pathology
5. Special Populations
Diagnostic challenges in pediatric, pregnant, and elderly patients.
Pediatric Considerations
- Higher perforation rates (15-30%)
- Ultrasound first-line (avoids radiation)
- Smaller diameter cutoff (>5.5mm)
Pregnancy Considerations
- Appendix displaced superiorly by gravid uterus
- Ultrasound first-line, MRI if indeterminate
- CT reserved for complex cases after 1st trimester
Elderly Considerations
- Atypical presentations common
- Higher perforation rates at presentation
- Increased malignancy risk as alternate diagnosis
Comparative Imaging Features
| Feature | Ultrasound | CT |
|---|---|---|
| Appendix diameter | >6mm non-compressible | >6mm |
| Wall thickening | >3mm with hyperemia | Enhancing wall |
| Periappendiceal inflammation | Hyperechoic fat | Fat stranding |
| Appendicolith | Echogenic with shadowing | Calcified focus |
| Perforation | Disrupted wall, abscess | Focal defect, extraluminal air |
References
- Pinto Leite N, Pereira JM, Cunha R, Pinto P, Sirlin C. CT evaluation of appendicitis and its complications: imaging techniques and key diagnostic findings. AJR Am J Roentgenol. 2005;185(2):406-417. doi:10.2214/ajr.185.2.01850406
- Doria AS, Moineddin R, Kellenberger CJ, et al. US or CT for Diagnosis of Appendicitis in Children and Adults? A Meta-Analysis. Radiology. 2006;241(1):83-94. doi:10.1148/radiol.2411050913
- Mostbeck G, Adam EJ, Nielsen MB, et al. How to diagnose acute appendicitis: ultrasound first. Insights Imaging. 2016;7(2):255-263. doi:10.1007/s13244-016-0469-6
- Kessler N, Cyteval C, Gallix B, et al. Appendicitis: evaluation of sensitivity, specificity, and predictive values of US, Doppler US, and laboratory findings. Radiology. 2004;230(2):472-478. doi:10.1148/radiol.2302021520
- Barger RL, Nandalur KR. Diagnostic performance of magnetic resonance imaging in the detection of appendicitis in adults: a meta-analysis. Acad Radiol. 2010;17(10):1211-1216. doi:10.1016/j.acra.2010.05.010
- Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology. 2000;215(2):337-348. doi:10.1148/radiology.215.2.r00ma24337
- van Randen A, Bipat S, Zwinderman AH, Ubbink DT, Stoker J, Boermeester MA. Acute appendicitis: meta-analysis of diagnostic performance of CT and graded compression US related to prevalence of disease. Radiology. 2008;249(1):97-106. doi:10.1148/radiol.2483071652
- Drake FT, Mottey NE, Farrokhi ET, et al. Time to Appendectomy and Risk of Perforation in Acute Appendicitis. JAMA Surg. 2014;149(8):837. doi:10.1001/jamasurg.2014.77
- Rosen MP, Ding A, Blake MA, et al. ACR Appropriateness Criteria® Right Lower Quadrant Pain-Suspected Appendicitis. J Am Coll Radiol. 2011;8(11):749-755. doi:10.1016/j.jacr.2011.07.010
- American Institute of Ultrasound in Medicine (AIUM). AIUM practice guideline for the performance of ultrasound examinations of the abdomen and/or retroperitoneum. J Ultrasound Med. 2021;40(7):E1-E16. doi:10.1002/jum.15607