Cirrhosis
Introduction
Cirrhosis refers to a difuse process characterized by fibrosis and the conversion of normal liver architecture into structurally abnormal nodules. Various insults can injure the liver, including viral infections, toxins, hereditary conditions, or autoimmune processes. With each injury, the liver initially forms scar tissue (fibrosis) without losing its function. After a chronic injury, most of the liver tissue becomes fibrotic, leading to loss of function and the development of cirrhosis.
Clinical presentation
The classic clinical presentation of cirrhosis is hepatomegaly, jaundice, and ascites. However, early serious liver injury may be present without any clinical clues and the disease may not be detected until liver damage is extensive. These early symptoms may include;
- Fatigue and weakness
- Loss of appetite or unexplained weight loss
- Pain in the upper right abdomen
- Nausea and/or vomiting
- Easy bruising or bleeding
- Itchy skin
- Redness on the palms of the hands
- Spider-like blood vessels on the skin
Ultrasound features
- Volume redistribution: In the early stages of cirrhosis the liver may be enlarged, whereas in advanced stages the liver is often small, with relative enlargement of the caudate lobe, let lobe, or both, compared with the right lobe. The ratio of caudate to right lobe (C/RL) of 0.65 is indicative for cirrhosis with a specificity of 100%
- Coarse heterogeneous echotexture. Loss of normal homogeneous pattern with increased parenchymal echogenicity
- Nodular surface: Irregular, bumpy contour (best seen with high-frequency probes). This correspond to presence of regenerating nodules and fibrosis. Specificity >90% for cirrhosis
- Regenerating nodules: Regenerating nodules tend to be isoechoic or hypoechoic with a thin, echogenic border that corresponds to fibrofatty connective tissue. Because regenerating nodules have a similar architecture to the normal liver, ultrasound have limited ability to detect them.
- Portal hypertension: Ascites, Splenomegaly and Varices
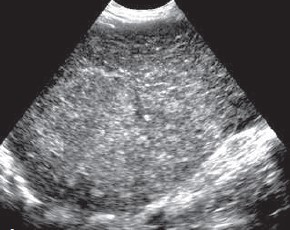
Coarse parenchyma and innumerable tiny, hyperechoic nodules

Volume redistribution
Sagittal image showing an enormous caudate lobe.

Small, end-stage livers with surface nodularity, best appreciated in patients with ascites, as shown here.
Key Diagnostic Criteria
- Nodular surface + coarse echotexture = 85% sensitivity
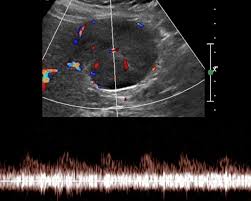
- Doppler findings increase diagnostic accuracy
- Early cirrhosis may have subtle or normal ultrasound findings
Doppler Ultrasound in Cirrhosis
Doppler assessment provides critical hemodynamic information:
| Vessel | Normal Findings | Cirrhosis Findings |
|---|---|---|
| Portal Vein | Hepatopetal flow (15-40 cm/s) | Slow flow (<15 cm/s), hepatofugal flow in advanced cases |
| Hepatic Artery | Resistive index (RI) 0.55-0.7 | RI >0.75 (due to increased arterial compensation) |
| Hepatic Veins | Phasic flow (reflects cardiac cycle) | Monophasic or flattened waveform (from fibrosis) |
Portal Vein Thrombosis
Present in 10-25% of cirrhotic patients. Look for:
- Echogenic material within portal vein
- Absent or partial flow on Doppler
- Cavernous transformation (chronic thrombosis)
Cirrhosis Complications on Ultrasound
Hepatocellular Carcinoma (HCC)
- Hypoechoic mass (most common)
- "Mosaic" pattern or capsule may be seen
- Internal vascularity on Doppler

Septated ascites
- Free fluid in peritoneal cavity
- Often in hepatorenal space and pelvis
- May show septations in infected ascites
LI-RADS Screening Protocol
For HCC surveillance in cirrhotic patients:
- Perform ultrasound every 6 months
- Targeted evaluation of any focal lesion >1 cm
- Multiphase CT/MRI for LI-RADS classification if suspicious
