Liver Ultrasound
Introduction
Liver ultrasound remains one of the most commonly performed abdominal imaging studies, offering a non-invasive, radiation-free method to evaluate hepatic anatomy and pathology. This comprehensive guide provides a systematic approach to liver ultrasound, covering essential technical aspects, normal anatomical features, and common pathological findings.
Liver anatomy
The liver is located in the right upper quadrant. It is almost completely covered by visceral peritoneum and is completely covered by a dense irregular connective tissue layer that lies deep to the peritoneum.
The liver is divided into two principal lobes (a large right lobe and a smaller left lobe) by the falciform ligament, a fold of the mesentery.
The falciform ligament extends from the undersurface of the diaphragm between the two principal lobes of the liver to the superior surface of the liver, helping to suspend the liver in the abdominal cavity.
In the free border of the falciform ligament is the ligamentum teres (round ligament), a remnant of the umbilical vein of the fetus; this fibrous cord extends from the liver to the umbilicus. The right and left coronary ligaments are narrow extensions of the parietal peritoneum that suspend the liver from the diaphragm.
Clinical Indications
Liver ultrasound is typically requested for the following clinical scenarios:
- Abnormal Liver Function Tests
- Evaluation of elevated ALT, AST, ALP, or bilirubin to assess for hepatitis, obstruction, or infiltrative diseases.
- Right Upper Quadrant Pain
- Investigation of biliary colic, cholecystitis, hepatitis, or other hepatic pathologies.
- Hepatomegaly
- Assessment of suspected liver enlargement detected on physical examination.
- Cancer Surveillance
- Screening for hepatocellular carcinoma in cirrhotic patients or those with chronic hepatitis.
- Suspected liver abscess.
- Jaundice
- Ascites
Technique/Preparation
The patient should take nothing by mouth for 8 hours preceeding the examination. If fluid is essential to prevent dehydration, only watre should be given. If the symptoms are acute, proceed with the examination
The liver is best examined with real-time sonography. Both supine and right anterior oblique positions should be used. Sagittal, transverse, coronal, and subcostal oblique views are suggested using both a standard abdominal transducer and a higherfrequency transducer.
In many patients, the liver is tucked beneath the lower right ribs, so a transducer with a small scanning face, allowing an intercostal approach, is invaluable.
Normal findings
The normal liver demonstrates characteristic sonographic features that serve as the baseline for identifying pathology.
Parenchymal Characteristics
- Echogenicity: Slightly hyperechoic compared to renal cortex
- Texture: Homogeneous fine granular pattern
- Margins: Smooth, well-defined capsular surface
- Size:
- Midclavicular line: ≤15.5 cm
- Midline: ≤13 cm
- Vasculature: Should be patent with no evidence of thrombosis or dilatation
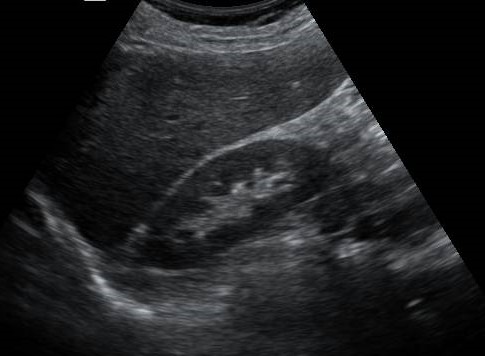
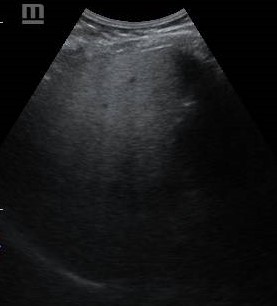
Normal liver
Homogeneous echopattern, smooth well-defined capsular surface and slightly hyperechoic to the right renal cortex
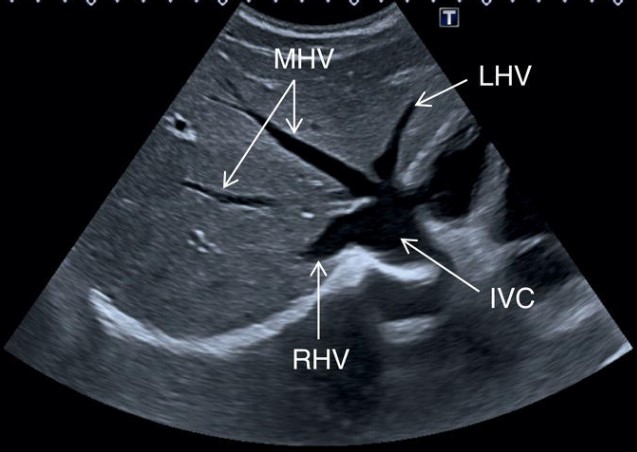
Normal hepatic vessels
The hepatic veins originate from the periphery of the liver, converging into the inferior vena cava (IVC). LHV, left hepatic vein; MHV, middle hepatic vein; RHV, right hepatic vein.
Key Diagnostic Points
- Always compare liver echotexture to the right kidney as an internal reference
- Measure liver size in both midclavicular and midline planes
- Assess all hepatic segments systematically
Common Pathological Findings
Diffuse Liver Disease
- 1. Fatty liver
- Appear as diffuse increase in hepatic echogenicity, impaired visualization of intrahepatic vessels and diaphragm, and poor penetration of posterior segment
- 2. Cirrhosis
- 3. Viral hepatitis
- In acute Hepatitis, the liver parenchyma may have a difusely decreased echogenicity, with accentuated brightness of the portal triads or periportal cuffing. Hepatomegaly and thickening of the gallbladder wall are associated findings. Most cases of chronic hepatitis are sonographically normal. When cirrhosis develops, sonography may demonstrate a coarsened echotexture and other morphologic changes of cirrhosis

Fatty liver
- Mild. Minimal difuse increase in hepatic echogenicity with normal visualization of diaphragm and intrahepatic vessel borders.

Fatty liver
- Moderate. Moderate difuse increase in hepatic echogenicity with slightly impaired visualization of intrahepatic vessels and diaphragm
Fatty liver
- Severe. Marked increase in echogenicity with poor penetration of posterior segment of right lobe of liver and poor or no visualization of hepatic vessels and diaphragm

Viral hepatitis
- Increased periportal cuffing giving a starry sky appearence of liver parenchyma
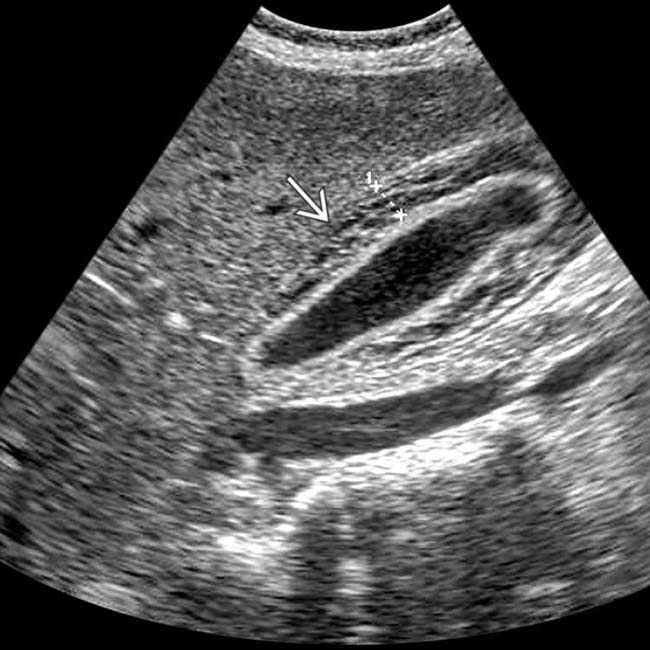
Viral hepatitis
- There is thickening of gallbladder wall (arrow)
Focal Liver Lesions
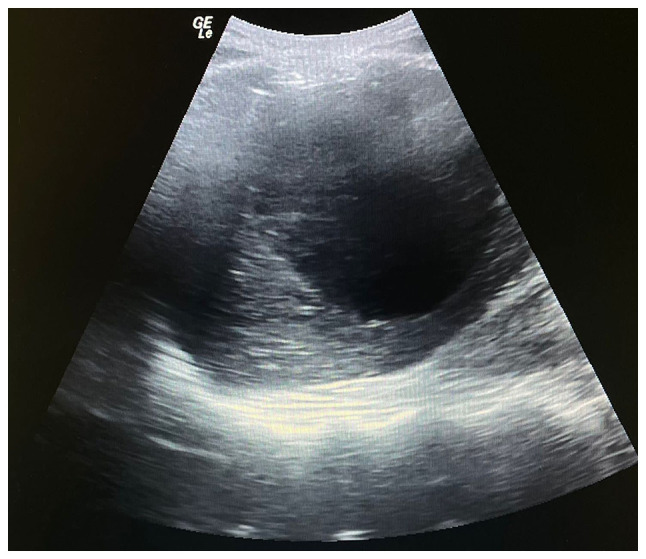
- 1. Liver Cysts
- Simple hepatic cysts are benign cysts which appear anechoic with a thin, well-demarcated wall and posterior acoustic enhancement. Complex hepatic cysts may show thick septae or nodules within the cyst. In this case, computed tomography is recommended because biliary cystadenomas and cystic metastases must be considered in the diferential diagnosis.
- 2. Peribiliary Cysts
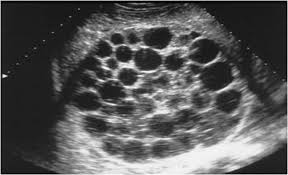
- 3. Autosomal Dominant Polycystic Disease
- 4. Biliary Hamartomas (von Meyenburg Complexes)
- 5. Liver abscess
- The abscess wall can vary from well defined to irregular and thick. They appear as cystic, with the fluid ranging from echo free to highly echogenic. Regions of early suppuration may appear solid with altered echogenicity, usually hypoechoic, related to the presence of necrotic hepatocytes. Echogenic foci with a posterior reverberation artifact due to gas-producing organisms
- 6. Candidiasis
- 7. Hydatid Disease
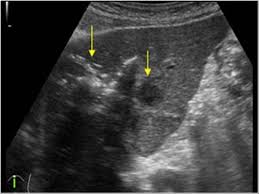
- These can present as a broad spectrum of sonographic findings; simple, centrally echo-free cyst with sharp outline and posterior acaustic enhacement, echo-free cyst containing fine internal debris due to hydatid sand, well-defined cystic mass with internal debris and membrane floating within the cyst, or complex cyst containing multiple internal cysts and doughter vesicles with echogenic materials filling some of the cysts and intervening spaces
- 8. Schistosomiasis
- 9. Glycogen Storage Disease (Glycogenosis)
- 10. Portal Hypertension

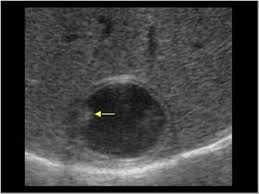
Simple hepatic cyst
- Thin and well-demarcated wall
- Posterior acoustic enhancement
Complex hepatic cyst
- Complex hepatic cyst with multiple thick septae
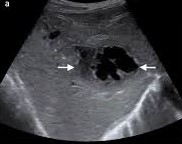
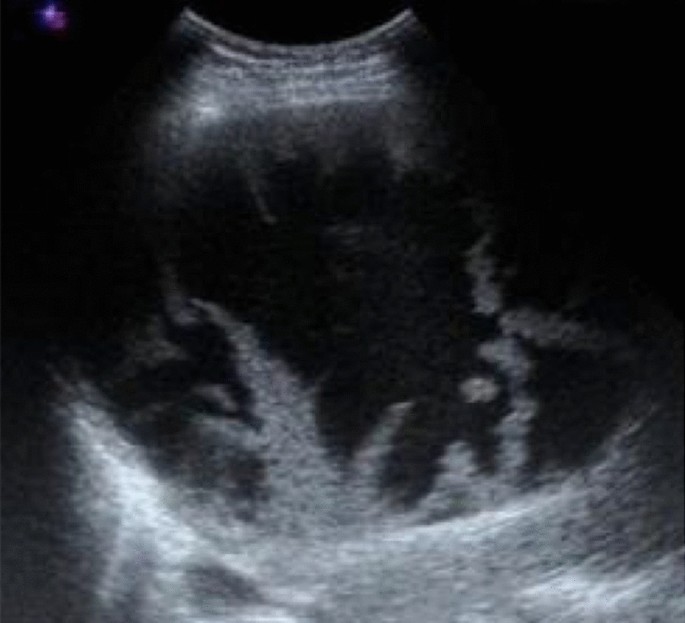
Liver abscess
- Anechoic, irregular, thick walled cystic liver mass
Liver abscess
- Echogenic foci with posterior reverberation artifacts
Liver abscess
- Liver cyst with internal echoes, representing an abscess
Hydatid cyst
- Simple echo-free cyst with double wall and fine internal debris.
Hydatid cyst
- Complex cyst containing doughter cysts

Hydatid cyst
- A well-defined cyst with internal floating membranes
Conclusion
Liver ultrasound remains an indispensable first-line imaging modality for evaluating hepatic pathology. A systematic approach assessing parenchymal echotexture, vascular patterns, and focal abnormalities enables accurate diagnosis of most hepatic conditions. While ultrasound excels as a screening tool, complementary imaging with contrast-enhanced ultrasound, CT, or MRI may be required for definitive characterization of certain lesions.
References
- American College of Radiology. ACR Appropriateness Criteria® for Right Upper Quadrant Pain. 2021.
- Dietrich CF, et al. EFSUMB Guidelines on Interventional Ultrasound. Ultraschall in Med. 2020.
- Khalili K, et al. Sonographic features of hepatocellular carcinoma. J Clin Ultrasound. 2019.
