Splenic trauma
Introduction
Splenic trauma is the most common abdominal injury in blunt trauma cases, accounting for approximately 25-30% of all blunt abdominal injuries. Focused Assessment with Sonography in Trauma (FAST) exam serves as the initial imaging modality of choice in hemodynamically unstable trauma patients due to its rapid, non-invasive, and repeatable nature.
Ultrasound technique
1. FAST exam protocal
- Use a curvilinear transducer (2-5 MHz)
- Patient in supine position (left lateral decubitus may help in stable patients)
- Place transducer in left upper quadrant at the posterior axillary line between 8th-11th ribs
- Angle transducer toward the spleen and diaphragm
- Evaluate the splenorenal recess (Morison's pouch equivalent on the left)
- Assess for free fluid and parenchymal abnormalities
2. Optimizing Imaging
- Use adequate acoustic coupling gel
- Apply gentle pressure to minimize rib shadows
- Adjust depth to include diaphragm and kidney
- Use harmonic imaging to reduce artifacts
- Compare with contralateral side when possible
Sonographic findings in splenic trauma
1. Direct Signs of Injury
- Parenchymal heterogeneity: Irregular areas of mixed echogenicity
- Lacerations: Hypoechoic or anechoic linear defects
- Hematomas: Hypoechoic or anechoic collections within parenchyma
- Subcapsular hematoma: Crescent-shaped fluid collection compressing spleen or a hypoechoic strip around the spleen
- Contour abnormalities: Irregular splenic outline
2. Indirect Signs
- Free fluid: Anechoic collections in splenorenal recess, perisplenic space, or pelvis
- Hemoperitoneum: May appear as complex fluid with internal echoes
- Perisplenic clot: Echogenic material adjacent to spleen
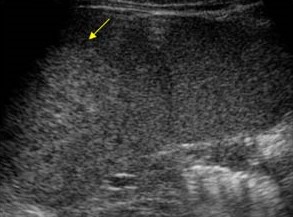
Parenchymal heterogeneity
- An irregular area of heterogeneous echotexture (Arrow)
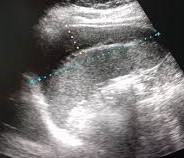
Subcapsular hematoma
- A large mostly hypoechoic subcapsular splenic collection.

Leceration
- Hypoechoic linear defects (arrows) within the spleen.

Hematoma
- Hypoechoic collection with the spleen

Perisplenic hematoma
- Coronal scan shows a hematoma (arrows) lateral to the spleen (s)
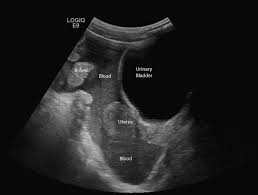
Hemoperitoneum
- Peritoneal fluid collection with echoes. Theis is an indirect sign of splenic trauma
Grading of splenic injuries
American Association for the Surgery of Trauma (AAST) Grading
- Subcapsular hematoma <10% surface area (Grade 1): Small crescentic hypoechoic area
- Subcapsular 10-50%, laceration <1cm depth (Grade 2): Moderate subcapsular fluid, small parenchymal defect
- Subcapsular >50%, laceration 1-3cm depth (Grade 3): Large subcapsular collection, obvious laceration
- Laceration >3cm or involving segmental vessels (Grade 4): Deep laceration, significant parenchymal disruption
- Shattered spleen or hilar vascular injury (Grade 4): Completely fragmented spleen, massive hemoperitoneum
Limitations and Pitfalls
- Lower sensitivity for small injuries without hemoperitoneum
- Difficult in obese patients or those with subcutaneous emphysema
- Cannot reliably assess for active bleeding
- May miss retroperitoneal hematomas
- Operator-dependent with variable expertise
When to Consider CT
- Negative FAST but high clinical suspicion
- Hemodynamically stable patients with suspected injury
- Characterization of injury extent for non-operative management
- Evaluation of associated injuries
Clinical Management Implications
Ultrasound findings in the trauma setting directly impact management:
Positive FAST (Free Fluid Present)
- Hemodynamically unstable: Likely emergent laparotomy
- Hemodynamically stable: CT for further characterization
Negative FAST (No Free Fluid)
- Low-risk patients: May avoid CT if low clinical suspicion
- High-risk patients: Still may require CT based on mechanism
Serial Examinations
In borderline cases, serial FAST exams (every 15-30 minutes) can detect delayed hemorrhage. Any clinical deterioration should prompt repeat ultrasound evaluation.
Conclusion
Ultrasound is an invaluable tool in the initial evaluation of splenic trauma, particularly in unstable patients where rapid diagnosis is critical. While it has limitations in sensitivity and precise injury characterization compared to CT, its speed, portability, and repeatability make it essential in trauma algorithms. Proper technique and recognition of both direct and indirect signs of splenic injury can significantly impact patient outcomes.
