Biliary Tree Ultrasound
Introduction
Ultrasound is the primary imaging modality for evaluating the biliary system due to its non-invasive nature, absence of ionizing radiation, real-time imaging capabilities, and widespread availability. It serves as the initial investigation for suspected biliary pathology with a sensitivity of 91-97% for detecting gallstones.
Anatomy of the biliary tree
The biliary system consists of a series of ducts that transport bile from the liver to the duodenum:
- Intrahepatic bile ducts: Follow portal triads (parallel to portal veins)
- Right and left hepatic ducts: Merge to form the common hepatic duct (CHD)
- Cystic duct: Connects gallbladder to CHD
- Common bile duct (CBD): Formed by union of CHD and cystic duct
Indications for Biliary Ultrasound
1. Common Clinical Scenarios
- Right upper quadrant (RUQ) abdominal pain
- Suspected cholelithiasis or choledocholithiasis
- Jaundice (obstructive vs. hepatocellular)
- Abnormal liver function tests (especially elevated ALP and GGT)
- Fever of unknown origin (screening for cholangitis)
2. Specific Clinical Indications
- Acute cholecystitis: RUQ pain + fever + leukocytosis
- Biliary obstruction: Jaundice + pruritus + pale stools
- Post-liver transplant: Monitor for biliary strictures
- Chronic liver disease: Evaluate for secondary biliary changes
Scanning Technique and Preparation
1. Patient Preparation
- Fasting: 6-8 hours (reduces bowel gas and gallbladder contraction)
- Positioning: Supine or left lateral decubitus (improves CBD visualization)
- Breathing instructions: Instruct patient to hold breath in expiration
2. Equipment Settings
- Transducer: Curvilinear (3-5 MHz) for adults, higher frequency for pediatrics
- Depth: Adjust to include entire biliary tree (typically 12-16 cm)
- Harmonic imaging: Reduces artifacts and improves resolution
- Focal zones: Set at level of porta hepatis
3. Systematic Scanning Approach
- Subcostal view: Identify gallbladder and portal triad
- Intercostal view: Assess intrahepatic ducts
- CBD tracing: Follow from porta hepatis to pancreatic head
- Color Doppler: Differentiate ducts from vessels
Normal Sonographic Findings
1. Gallbladder
- Pear-shaped anechoic structure
- thickness <3 mm
- No internal echoes (except dependent sludge)
- Normal length 7-10 cm, width <4 cm
2. Bile Ducts
- Walls appear as thin echogenic lines
- Lumen is anechoic
- No intraductal masses or calculi
- No periductal edema or vascularity
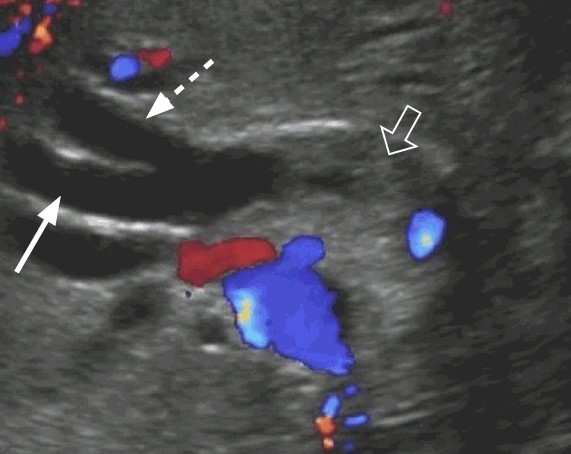
Landmark: Portal Triad
The "Mickey Mouse" sign represents the portal triad in cross-section:
- Head: Hepatic artery (smallest)
- Left ear: Common bile duct
- Right ear: Portal vein (largest)

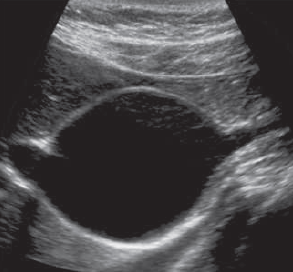
Normal gallbladder
Thin-walled (typically less than 3mm thick), anechoic (appears dark or black) structure that is pear-shaped and measures around 7-10cm in length and 3-4cm in width
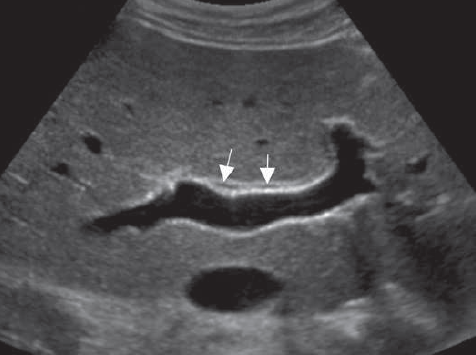
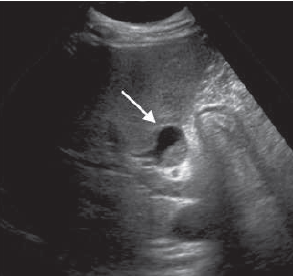
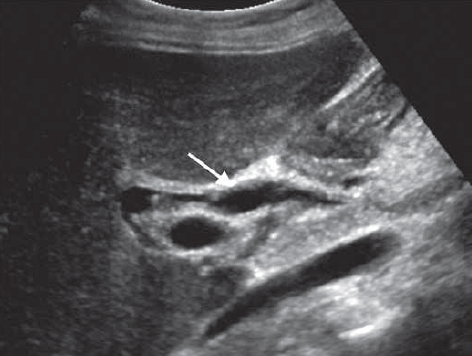
Normal Bile Ducts
Right and left hepatic ducts (short arrows) are normally seen lying anterior to the portal veins. Appear anechoic without any signs of dilation or obstruction
Pathological Findings
1. Cholelithiasis (Gallstones)
- Findings: Mobile hyperechoic focus with posterior shadowing
- WES triad: Wall-echo-shadow in contracted gallbladder
- Complications: Cholecystitis, empyema, porcelain gallbladder
2. Choledocholithiasis (CBD Stones)
- Findings: Echogenic intraluminal focus with shadowing
- Dilation: CBD >6 mm with proximal ductal dilation
- Twinkling artifact: May be seen on color Doppler
3. Biliary Obstruction
- Intrahepatic: "Too many tubes" sign (multiple dilated ducts)
- Extrahepatic: "Double barrel" sign (dilated CBD + portal vein)
- Causes: Stones (75%), tumors (20%), strictures (5%)
4. Cholangitis
- Findings: Ductal dilation + wall thickening + intraluminal debris
- Clinical: Charcot's triad (fever, jaundice, RUQ pain)
5. Choledochal Cysts
- Type I: Fusiform dilation of the CBD, are the most common (80%)
- Type II: Are true diverticula of the bile ducts and are very rare
- Typr III: The “choledochoceles,” are confined to the intraduodenal portion of the CBD
- Type IV:
- Type IVa: Cysts are multiple intrahepatic and extrahepatic biliary dilations
- Type IVb: Cysts are confined to the extrahepatic biliary tree.
- Type V: Caroli disease has been classiied as a type V cyst. However, it has a diferent embryonic origin and is not a true choledochal cyst.
6. Caroli Disease. A rare congenital disorder characterized by segmental, non-obstructive dilation of intrahepatic bile ducts. Caroli disease leads to saccular dilation or, less often, fusiform dilation of the intrahepatic biliary tree, resulting in biliary stasis, stone formation, and bouts of cholangitis and eventually sepsis. Unlike recurrent pyogenic cholangitis, the ductal contents do not form a cast of the dilated system and thus are more easily identiied as ductal contents.
7. Mirizzi Syndrome. A rare complication of chronic gallstone disease where extrinsic compression of the common hepatic duct (CHD) occurs due to; an impacted gallstone in the cystic duct/gallbladder neck or Secondary inflammation/fibrosis causing biliary obstruction
- Dilated CHD & intrahepatic ducts above the level of obstruction (normal CBD below)
- Impacted stone - Hyperechoic focus with shadowing in gallbladder neck/cystic duct
- Wall thickening - Gallbladder/cystic duct wall >3mm with edema
- "Parallel channel" sign - Dilated CHD adjacent to portal vein
- Gallbladder contraction - Small, shrunken gallbladder
- Pericholecystic inflammation - Hyperechoic fat, fluid collections
- Liver parenchyma changes - Possible edema near porta hepatis
8. Hemobilia. This is due to iatrogenic biliary trauma mostly caused by percutaneous biliary procedures or liver biopsies, cholangitis or cholecystitis, vascular malformations or aneurysms, abdominal trauma, and malignancies. The appearance of blood within the biliary tree is similar to blood clots encountered elsewhere; Most oten, the clot is echogenic or of mixed echogenicity, and retractile, conforming to the shape of the duct. Occasionally, hemobilia may appear tubular with a central hypoechoic area. Acute hemorrhage will appear as fluid with low-level internal echoes. Blood clots may be mobile. Extension into the gallbladder is common.
9. Pneumobilia. Refers to air within the biliary tree, most commonly caused by; Post-surgical states (e.g., sphincterotomy, biliary-enteric anastomosis), Biliary-enteric fistulas (e.g., gallstone ileus), Infection (emphysematous cholecystitis/cholangitis) or Iatrogenic (ERCP, stent placement). Air in the bile ducts has a characteristic appearance. Bright, echogenic linear structures following the portal triads are seen, more oten in a nondependent position. Posterior “dirty” shadowing, reverberation, and ring-down artifacts are seen with large quantities of air. Movement of the air bubbles, best seen just ater changing the patient’s position, is diagnostic.
- Acute (Bacterial, Ascending) Cholangitis
- Liver Flukes
- Recurrent Pyogenic Cholangitis
- Ascariasis
- HIV Cholangiopathy
11. Immune-Related Diseases of the Biliary Tree
- Primary Biliary Cirrhosis and Autoimmune Cholangitis
- Primary Sclerosing Cholangitis
- IgG4-Related Cholangitis
12. Cholangiocarcinoma
- Intrahepatic Cholangiocarcinoma
- Hilar Cholangiocarcinoma
13. Metastases to Biliary Tree. Metastases to the biliary tree mimic the varied appearance of cholangiocarcinoma, affecting both the intrahepatic and extrahepatic ducts. The history of past or concurrent malignancy along with multiple lesions should suggest metastases. In our experience the breast, colon, and skin (melanoma) constitute the primary sites of malignancy.
Critical Findings Requiring Urgent Intervention
The "Mickey Mouse" sign represents the portal triad in cross-section:
- CBD stone with cholangitis (emergency ERCP needed)
- Gallbladder empyema (risk of perforation)
- Biliary-enteric fistula (pneumobilia present)

Cholelithiasis
- Mobile hyperechoic focus with posterior shadowing.

WES triad
- Wall echo shadow in a contracted gallbladder
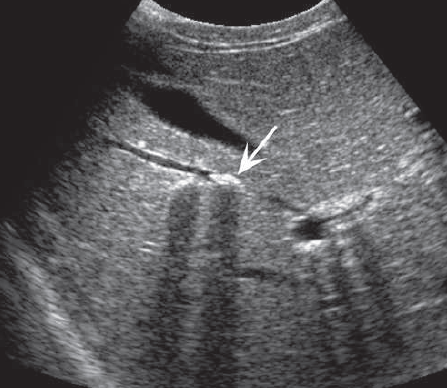
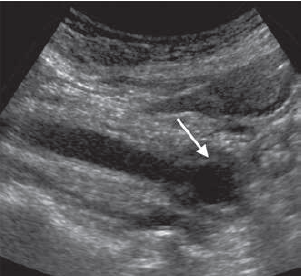
Choledocholithiasis
- Small stones (arrow) are seen in the right liver lobe causing acoustic shadowing. Note the dilated duct proximal to the larger stone.
Choledocholithiasis
- Common bile duct (CBD) stones. Small stone (arrow) may not show shadowing
Biliary obstruction
- Intrahepatic (dilated bile ducts)

Biliary obstruction
- Extrahepatic - Double barrel" sign (dilated CBD + portal vein)
Choledochal cyst - Type I
- Fusiform dilation of the common bile duct (CBD) is seen, but no obstructive lesion is noted.
Choledochal cyst - Type II
- A large diverticulum (arrow) arising from the common hepatic duct at the portal hepatis and containing mobile debris.
Choledochal cyst - type III
- Fusiform dilation of the distal CBD (arrow) is demonstrated protruding into the duodenum.
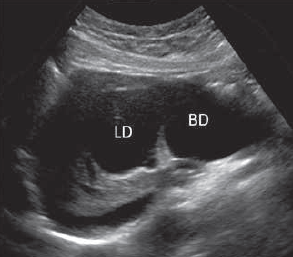
Choledochal cyst - type IV
- Sagittal view of the liver shows a markedly dilated bile duct (BD) and left hepatic duct (LD).
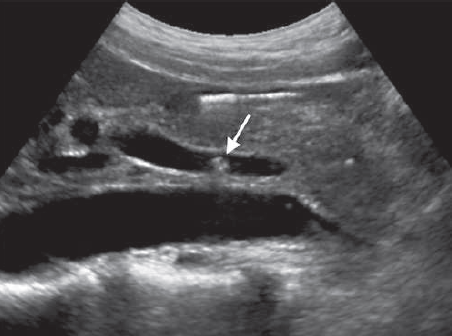
Cholangitis
- Bile duct wall thickening (arrow) in a dilated duct.

Caroli disease
- Oblique image through the right lobe of the liver demonstrates dilated ducts with sacculations typical of Caroli disease..
Conclusion
Ultrasound remains the first-line imaging modality for biliary tree evaluation, offering excellent diagnostic accuracy for common conditions like cholelithiasis and biliary obstruction while avoiding radiation exposure. Proper technique including patient preparation, transducer selection, and systematic scanning approach is essential for optimal results.
While ultrasound has limitations in evaluating the distal CBD (particularly with overlying bowel gas), it provides crucial initial information that guides further management decisions regarding the need for advanced imaging (MRCP) or therapeutic interventions (ERCP).
References
- American College of Radiology (ACR). (2022). ACR Appropriateness Criteria® Right Upper Quadrant Pain. Journal of the American College of Radiology, 19(5S), S223-S231.
- Middleton, W. D., Kurtz, A. B., & Hertzberg, B. S. (2021). Ultrasound: The Requisites (4th ed.). Elsevier.
- Rumack, C. M., Levine, D. (2022). Diagnostic Ultrasound (6th ed.). Elsevier.
- European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB). (2020). Guidelines on Interventional Ultrasound (INVUS), Part III - Abdominal Treatment Procedures. Ultraschall in der Medizin, 41(1), 16-44.
- National Institute for Health and Care Excellence (NICE). (2021). Gallstone disease: diagnosis and management. NICE Clinical Guideline 188.
