Spleen Ultrasound
Introduction
The spleen and left upper quadrant (LUQ) should be routinely evaluated on all abdominal investigations, especially in patients with suspected splenomegaly, LUQ pain, or trauma. In general, the spleen can be examined by ultrasound without dificulty. As part of abdominal ultrasound examinations or as a focused assessment, spleen ultrasound provides valuable diagnostic information with high patient tolerance and relatively low cost. Because the normal spleen is uniform in echogenicity, focal abnormalities stand out clearly. Similarly, perisplenic abnormalities and fluid collections are usually easily identified. Occasionally, because the spleen is located high in the LUQ, dificulties can be encountered. Shadowing from ribs, overlying bowel gas, and overlying lung can obscure visualization of the deeper structures. Expertise and persistence may be required to overcome these obstacles
Anatomy of the spleen
The normal adult spleen is convex superolaterally and concave inferomedially. The spleen lies between the fundus of the stomach and the diaphragm, with its long axis in the line of the let 10th rib. The diaphragmatic surface is in contact with the diaphragm and the rib cage, its is convex and is usually situated between the 9th and 11th ribs. The visceral or inferomedial surface is in contact with other abdominal viscera and has gentle indentations where it comes into contact with the stomach, left kidney, pancreas, and splenic flexure.
Anatomical relations
- Anterior: Stomach
- Posterior: Diaphragm, Left lung and Rib 9 - 11
- Infereior: Left colic flexure (splenic flexure)
- Medial: Left kidney and Tail of the pancreas
Clinical Indications
Ultrasound is particularly valuable for:
- Evaluating splenomegaly (enlarged spleen)
- Assessing traumatic injuries
- Detecting focal lesions (cysts, tumors, abscesses)
- Monitoring known splenic pathology
- Guiding interventional procedures
Technique/Preparation
Patient preperation. The patient should take nothing by mouth for 8 hours preceeding the examination. If fluid is essential to prevent dehydration, only water should be given. If symptoms are acute, proceed with the examination. Infants - clinical condition permiting - should be given nothing by mouth for 3 hours preceeding the examination.
For acutely ill patients (e.g trauma, sudden abdominal pain, post surgical pyrexial), no preperation is needed.
Position of the patient. The patient should be supine initially and later on the right side.
Sonographic technique. The most common and easy approach to visualize the spleen is to maintain the patient in the supine position and place the transducer in the coronal plane of section posteriorly in one of the lower left intercostal spaces. The patient can then be examined in various degrees of inspiration to maximize the window to the spleen. A modest inspiration depresses the central portion of the left hemidiaphragm and spleen inferiorly so that they can be visualized. The plane of section should then be swept posteriorly and anteriorly to view the entire volume of the spleen.
Normal findings
Parenchymal Characteristics
- Echogenicity: Homogeneous, slightly hypoechoic compared to liver
- Echotexture: Fine, uniform granular pattern
- Capsule: Thin, hyperechoic line surrounding the organ
Vascular Structures
- Splenic vein: Anechoic tubular structure at the hilum (normal diameter 5-10 mm)
- Splenic artery: Pulsatile Doppler signal at the hilum
- Intrasplenic vessels: Normally not visible unless using power Doppler
Normal Variants
- Accessory spleen(s): Small (1-3 cm) round structures with identical echotexture to main spleen (20% of population)
- Splenic clefts: Linear indentations on the surface (may mimic lacerations)
- Splenunculi: Larger accessory spleens (may be ectopic)

Normal spleen
- Homogeneous, fine and uniform granular pattern
- Thin, hyperechoic capsule surrounding the organ
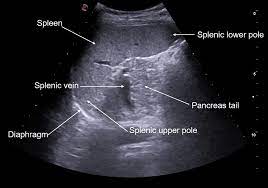
Normal spleen
Splenic vein and the anatomical relations of the spleen
Technical tip: Have the patient take a deep breath and hold it to bring the spleen down below the costal margin for better visualization.
Common pathological findings
- Splenomegaly: Craniocaudal length >13 cm in adults. Ultrasound may show rounded splenic contour, extension of the spleen below the left costal margin and medial displacement of the left kidney
- Splenic cysts
- Nodular splenic lesions: Nodular lesions are often multiple. If splenic nodules are present in a patient with a known diagnosis such as lymphoma, tuberculosis, or sarcoidosis, these nodules likely represent the same disease. However, if no diagnosis has been established and the splenic nodules are an isolated finding, the diagnosis is rarely made on the imaging features alone. The most common causes of splenic nodules include infection (e.g., mycobacteria, histoplasmosis), sarcoidosis, and malignancy
- Hemangioma: Are the most common primary benign neoplasm of the spleen. They are usually isolated phenomena but can be part of a generalized condition, such as hemangiomatosis or Klippel-Trenaunay-Weber syndrome. The lesions often have a well-defined echogenic appearance similar to the typical appearance of hemangiomas in the liver,
- Sicke cell disease: Sickle cell disease almost always affects the spleen. The most common splenic complications are autosplenectomy, acute sequestration, hypersplenism, massive infarction, and abscess.
- Gaucher disease: In Gaucher disease, splenomegaly occurs almost universally, and approximately one-third of patients have multiple splenic nodules. These nodules frequently are well-defined hypoechoic lesions, but they may also be irregular, hyperechoic, or of mixed echogenicity. Pathologically, these nodules represent focal areas of Gaucher cells associated with ibrosis and infarction. In rare cases, the entire spleen may be involved, with ultrasound showing a difuse heterogeneous spleen.
- Gamna-Gand bodies: Gamna-Gandy bodies (Gamna nodules) are fibrosiderotic nodules that result from organized focal hemorrhagic infarcts, typically seen in congestive splenomegaly and sickle cell disease. Gamna-Gandy bodies appear as multiple punctate hyperechoic foci on ultrasound but are usually better seen on MRI.
-
Congenital abnormalities
- Accessory spleens, also known as splenunculi, are common normal variants found in up to 30% of autopsies. They are typically located near the splenic hilum and have similar echogenicity as the normal spleen. Splenunculi may be confused with enlarged lymph nodes around the spleen or with masses in the tail of the pancreas. When the spleen enlarges, the accessory spleens may also enlarge.
- Ectopic accessory spleens, described in various locations, including the pancreas and scrotum, are typically confused with abnormal masses or, in rare cases, can undergo torsion and cause acute abdominal pain. The vast majority of accessory spleens, however, are easy to recognize sonographically as small, rounded masses, usually less than 5 cm in diameter, with the same echogenicity as the spleen (Fig. 5.33). CT, MRI, or, in challenging cases, scintigraphy with technetium-labeled heat-damaged red blood cells, can conirm the diagnosis.
- A “wandering spleen” (or mobile spleen) can be found in unusual locations and may be mistaken for a mass. It is caused by absence or extreme laxity of the supporting ligaments and a long, mobile mesentery. The mobile spleen may undergo torsion, resulting in acute or chronic abdominal pain. If the diagnosis of a wandering spleen is made in a patient with acute abdominal pain, the diagnosis of torsion is supported by color flow Doppler imaging showing absence of blood low.
-
Splenic trauma
- Laceration: Linear hypoechoic or anechoic defect
- Hematoma: Irregular hypoechoic collection (may evolve in echogenicity)
- Subcapsular hematoma: Crescentic fluid collection compressing parenchyma
- Free fluid: Blood in perisplenic space or Morrison's pouch
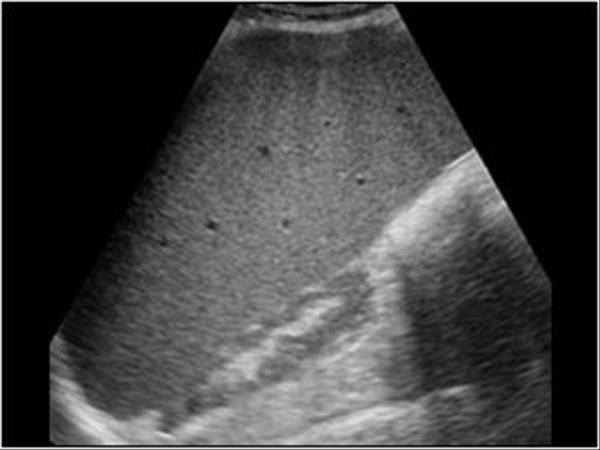
Splenomegaly
- Splenomegaly with compression of the left kidney
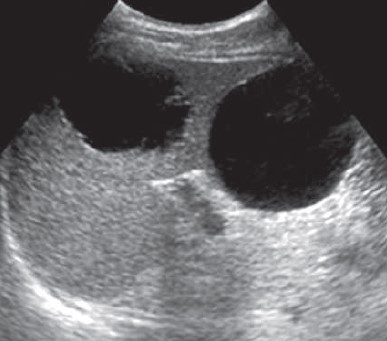
Splenic cysts
- Central 5-cm cyst with irregular borders and a simple 6-cm cyst at the inferior portion of the spleen. Both congenital cysts and pseudocysts may have this appearance.
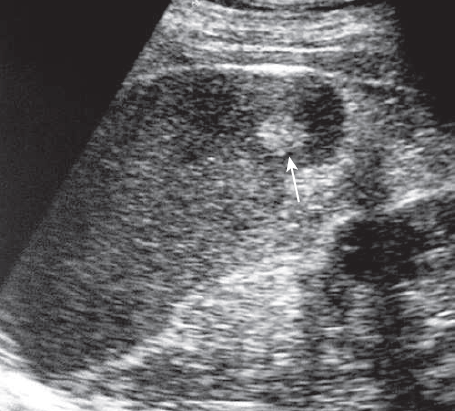
Hemangioma
- Well-deined, rounded, echogenic lesion (arrow) is similar to the typical liver hemangiomas.

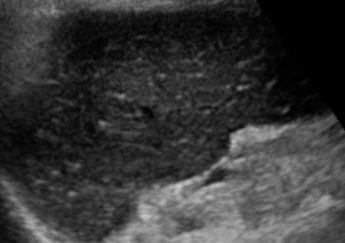
Splenic infarct
- Coronal image shows a well-deined hypoechoic central area reaching the splenic capsule medial and lateral in a patient with sickle cell disease, in keeping with splenic infarct
Gaucher disease
- Enlarged spleen containing a 2-cm heterogeneous nodule
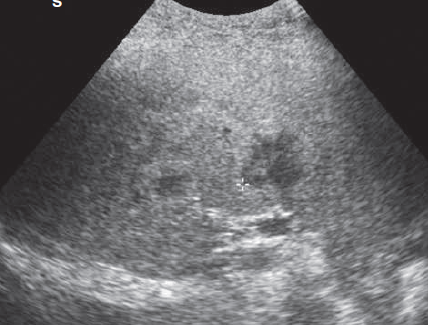
Gamna Gandy bodies
- The spleen shows multiple tiny echogenic foci without acoustic shadowing diffusely involving the parenchyma. These are siderotic nodules or Gamna-Gandy nodules
Documentation and reporting
A comprehensive spleen ultrasound report should include:
- Technical Factors:
- - Patient position(s) used
- - Transducer frequency
- - Views obtained
- Findings:
- - Spleen size (3 dimensions when possible)
- - Parenchymal echogenicity and echotexture
- - Presence of focal lesions (size, location, characteristics)
- - Vascular patency (when evaluated)
- - Surrounding structures (left kidney, pancreas tail)
- - Presence of free fluid
- Impression:
- - Summary of key findings
- - Correlation with clinical history when available
- - Recommendations for further imaging if needed
References
- Rumack CM, Wilson SR, Charboneau JW, Levine D. Diagnostic Ultrasound. 5th ed. Elsevier; 2018.
- American Institute of Ultrasound in Medicine (AIUM). Practice Parameter for the Performance of an Ultrasound Examination of the Abdomen and/or Retroperitoneum. 2020.
- Dietrich CF, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part III - Abdominal Treatment Procedures (Long Version). Ultraschall in der Medizin 2016;37(1):27-59.
- Nino-Murcia M, Jeffrey RB Jr. Imaging the patient with right upper quadrant pain. Semin Roentgenol 2001;36(2):81-91.
- Gorg C. The forgotten organ: contrast enhanced sonography of the spleen. Eur J Radiol 2007;64(2):189-201.
- Kessler N, et al. Evaluation of the spleen with ultrasound: normal and pathological findings. J Radiol 2004;85(4 Pt 2):655-63.
- Paterson A, et al. A pattern-oriented approach to splenic imaging in infants and children. Radiographics 2009;29(5):1465-85.
